It is widely accepted and recognized that psychodermatologic issues are commonly encountered in dermatological practices. There is evidence to suggest taking a more holistic approach can be hugely beneficial to patients and that practitioners can find value from more in-depth knowledge of psychodermatology.
Coping with the negative impacts of chronic skin disease can be severely distressing. Conditions such as eczema, psoriasis, acne, alopecia, and rosacea manifest physically and cause significant emotional and mental anguish for patients.
Many people are extremely self-conscious of their skin condition and prefer to remain covered up to avoid stares and whispers. The emotional turmoil, feelings of rejection, and despair force many individuals to withdraw from social interaction altogether, further deteriorating their emotional and mental state.
According to board-certified dermatologist Lauren Karpinski, MD,
“Many individuals with chronic skin diseases report having been asked to leave public places such as a community recreation center or pool when their condition was mistaken for something contagious.”
Lauren Karpinski, MD
These stigmas and rejection play a significant role in creating feelings of distress, anxiety, and lowered self-esteem.
The Mind and Skin Connection
It is believed that approximately 30-40% of patients presenting with dermatologic conditions also experience psychiatric disorders. A study of 526,808 adults with atopic eczema revealed those with this skin disease were more likely to develop new depression and anxiety. A further 2014 National Rosacea Society survey of 1,675 patients with rosacea found that 90% of respondents reported lowered self-esteem and self-confidence, 54% reported anxiety and helplessness, and 43% felt depressed. More than half of these patients stated that they avoided face-to-face contact. Another study conducted on out-patients from 13 European countries found a significantly higher prevalence of clinical depression, anxiety disorder, and suicidal ideation among patients with common skin diseases compared with controls.
It is a vicious circle in which stress, depression, and other kinds of psychological problems exacerbate existing skin problems.
"The common dermatological issues that have been documented to be made worse by stress include acne, rosacea, psoriasis, itching, eczema, pain, and hives, just to name a few."
Richard Fried, MD, PhD, board-certified dermatologist, and clinical psychologist
The Role of Psychodermatology
Psychodermatology, also known as psychocutaneous medicine, holds an important place in the dermatologic industry. It offers patients and providers optimal outcomes for the management and treatment of their debilitating physical and mental conditions.
By examining the crucial link between skin and mental health, psychodermatology aims to bridge the gap between skin diseases and psychiatric disorders. Incorporating key specialties such as dermatology, psychiatry, and psychology helps promote a holistic approach to these psychodermatoses.
Psychodermatologic disorders are generally classified into four categories:
Psychophysiologic disorders are associated with skin problems that are exacerbated by emotional stressors. These are not directly connected to the mind but stem from conditions that patients report worsening when under stress, such as eczema, acne, atopic dermatitis, and psoriasis.
Primary psychiatric disorders involve psychiatric conditions. There is no actual skin disease, but instead, self-induced cutaneous manifestations such as trichotillomania and delusions of parasitosis are present.
Secondary psychiatric disorders are associated with disfiguring skin disorders that patients may develop in response to their skin disease. Psychological problems such as depression or decreased self-esteem are commonly experienced.
Cutaneous sensory disorders are sometimes thought of as a miscellaneous category but include dysesthesias and unpleasant sensations such as stinging, burning, or itching without any clear etiology.
Supporting Further Education and Research
The Association for Psychoneurocutaneous Medicine of North America (APMNA), dedicated to the awareness of psychoneurocutaneous medicine, is made up of dermatologists, psychiatrists, psychologists, and allied health professionals dedicated to the study of the skin and mind connection.
Despite the widespread recognition that skin conditions can play a direct role in a patient’s mental health, practitioners lack a certain degree of familiarity and competence to properly handle these situations. While it is believed that psychodermatology is key in addressing the management of psychodermatological problems, there remains a need for further research and education in the field.
Speaking of managing the mental side of skin disorders, Dr. Fried has previously mentioned that a referral to a psychodermatologist or mental health professional with an interest in dermatologic manifestations can help some patients. However, at other times, treatment can be as simple as regular visits to their dermatologist, who can “assuage some of the ‘terror of chronicity and progression’ that they feel.
That being said, many believe that for effective referrals to take place, there must first be a level of trust between the patient and provider.
Board-certified dermatologist, Gina Caputo, DO, states,
“It is crucial that dermatologists identify these overlapping situations because psychodermatological patients often refuse a psychiatry referral. Oftentimes, recommending a referral before trust is formed can make the patient feel isolated and make the condition worse.”
Gina Caputo, DO
Evaluating any underlying psychiatric component of a skin disorder involves several elements. Establishing a good patient-provider relationship is key, where patients are open and honest and can discuss their issues freely is vital.
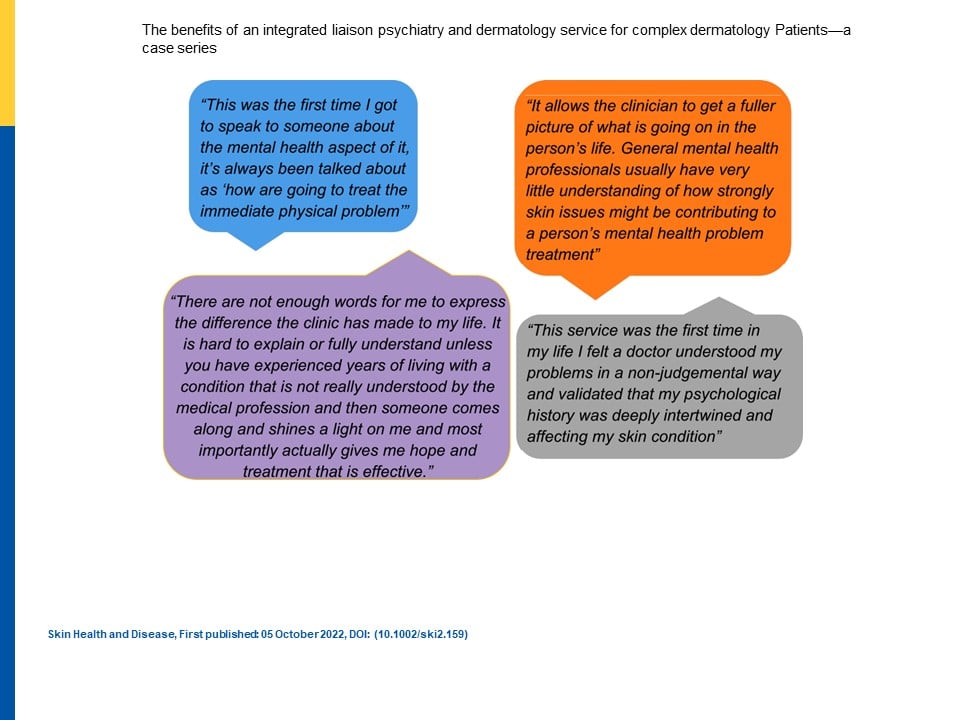
A recent pilot of an integrated service of a consultant dermatologist and a liaison psychiatrist providing coordinated care to complex psychodermatology patients reported positive results and optimistic patient feedback. In this U.K. study which took place over six months, 57 patients were examined by a dermatologist, and 33 of these were referred to a psychiatrist. Some of the patient responses to this integrated service are shown below.
The study reiterated the point from the U.K. National Health Service ‘Getting it Right the First Time’ report, which suggested improved access and expansion in psychodermatology services.
Key Takeaway
Research finds that dermatologists could greatly benefit from having a clearer understanding of the interaction between the skin and the patient’s emotional complaints. Recognizing any emotional or mental concerns as part of the overall clinical diagnosis can greatly improve treatment and support options for the patient.
Ultimately, psychodermatoses are a vicious cycle, and by helping one set of ailments, it is possible to help the other. As Dr. Fried states, “These kinds of interventions don’t just help patients’ distress. They can also improve patients’ skin and their responsiveness to treatment.”
- Ghosh S, Behere RV, Sharma P, Sreejayan K. Psychiatric evaluation in dermatology: an overview. Indian J Dermatol. 2013;58(1):39-43.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3555371/#ref5
- Yochai Schonmann, Kathryn E. Mansfield, Joseph F. Hayes, Katrina Abuabara, Amanda Roberts, Liam Smeeth, Sinéad M. Langan, Atopic Eczema in Adulthood and Risk of Depression and Anxiety: A Population-Based Cohort Study, The Journal of Allergy and Clinical Immunology: In Practice, 2020;8(1):248-257. https://www.sciencedirect.com/science/article/pii/S2213219819307536
- John Koo, M.D., And Andrew Lebwohl, Psychodermatology: The Mind and Skin Connection, Am Fam Physician. 2001;64(11):1873-1879. https://www.aafp.org/pubs/afp/issues/2001/1201/p1873.html#:~:text=Psychodermatology%2C%20or%20psychocutaneous%20medicine%2C%20focuses,optimal%20management%20of%20psychodermatologic%20disorders.
- Catherine MaiKhanh Nguyen, BS, Melissa Danesh, BS, Kourosh Beroukhim, BS, Eric Sorenson, BS, Argentina Leon, MD, and John Koo, MD, Psychodermatology: A Review, May 2015. Practical Dermatology. https://practicaldermatology.com/articles/2015-may/psychodermatology-a-review
- More Than Skin Deep: The Link Between Skin Health and Mental Health. https://www.apexskin.com/2022/03/23/skin-health-and-mental-health/
- Rebecca A. Clay, The link between skin and psychology, 2015;46(2):56. https://www.apa.org/monitor/2015/02/cover-skin
- http://www.psychodermatology.us/
- Dalgard FJ, Gieler U, Tomas-Aragones L, Lien L, Poot F, Jemec GBE, Misery L, Szabo C, Linder D, Sampogna F, Evers AWM, Halvorsen JA, Balieva F, Szepietowski J, Romanov D, Marron SE, Altunay IK, Finlay AY, Salek SS, Kupfer J. The psychological burden of skin diseases: a cross-sectional multicenter study among dermatological out-patients in 13 European countries. J Invest Dermatol. 2015;135(4):984-991. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378256/
- Azambuja RD. The need of dermatologists, psychiatrists and psychologists joint care in psychodermatology. An Bras Dermatol. 2017;92(1):63-71. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5312181/
- Bianca Nogrady, Manage the mental side of skin disorders, May 2013. https://www.mdedge.com/psychiatry/article/58776/somatic-disorders/manage-mental-side-skin-disorders
- Gina M. Caputo, D.O., Psychodermatology: Where the Skin and Mind Meet. June 2019. https://www.dermatologytimes.com/view/psychodermatology-where-skin-and-mind-meet
- Mohammad Jafferany, MD, Psychodermatology: When the Mind and Skin Interact, December 2011. https://www.psychiatrictimes.com/view/psychodermatology-when-mind-and-skin-interact
- Victoria Roberts,Jonathan Chan,Jo Davies,Janet Angus, The benefits of an integrated liaison psychiatry and dermatology service for complex dermatology Patients—a case series, October 2022. https://onlinelibrary.wiley.com/doi/full/10.1002/ski2.159
- GIRFT recommendations address dermatology workforce shortages and call for wider use of technology. https://www.gettingitrightfirsttime.co.uk/wp-content/uploads/2021/11/Dermatology-overview.pdf