In the U.S, approximately 9.6 million children under 18 years of age have atopic dermatitis (AD). In one-third of these cases, the disease presents as moderate to severe, placing a significant burden on patients, families, and caregivers.
The condition alone can be debilitating, but when accompanied by various comorbidities, AD can be quite a serious challenge for the patient and those tasked to care for them.
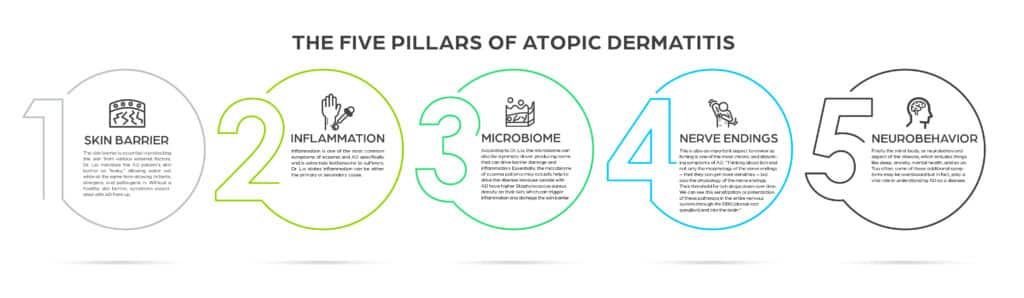
Founding director of the Chicago Integrative Eczema Center, Peter A. Lio, MD, weighs in on what he refers to as the five pillars of AD, stating that learning more about the ways these elements work together has helped to shape and refine our understanding of the disease.
The Five Pillars
The skin barrier is essential in protecting the skin from various external factors. Dr. Lio mentions the AD patient’s skin barrier as “leaky”, allowing water out while at the same time allowing irritants, allergens, and pathogens in. Without a healthy skin barrier, symptoms associated with AD flare up.
Inflammation is one of the most common symptoms of eczema and AD specifically and is extremely bothersome to sufferers. Dr. Lio states inflammation can be either the primary or secondary cause.
According to Dr. Lio, the microbiome can also be a primary driver, producing toxins that can drive barrier damage and inflammation. Essentially, the microbiome of eczema patients may actually help to drive the disease because people with AD have higher Staphylococcus aureus density on their skin, which can trigger inflammation and damage the skin barrier.
This is also an important aspect to review as itching is one of the most chronic and disturbing symptoms of AD.
Finally the mind-body, or neurobehavioral aspect of the disease, which includes things like sleep, anxiety, mental health, and so on. Too often, some of these additional symptoms may be overlooked but in fact, play a vital role in understanding AD as a disease.
Treatment Landscape
According to Dr. Lio, one of the main challenges to treatment in pediatric patients is a fear of the side effects. Some parents are anxious about certain medications and tend to put off starting treatment. Many also hope their children will eventually “grow out” of it. And while this may be true for some, many will maintain the disease into adulthood.
Dr. Lio, who is also a clinical assistant professor of dermatology and pediatrics at Northwestern University, Finebrook School of Medicine is a fan of the “therapeutic ladder,” starting on the lowest rung and working up from there. In many cases, patients may just need a good skincare routine, with moisturizing, cleansing, and avoiding known triggers.
Others, however, may require a more medical approach, which is where he would start with topical corticosteroids.
For those that don’t, that would be when to move up to the next rung on the ladder, with a more proactive approach and maintenance therapies. After that, he mentions, is when you would bring out the “big guns.” meaning the systemic therapies, biologic agents, phototherapy, and most recently, JAK inhibitors.
Fortunately, the AD treatment landscape continues to expand as more and more novel therapies for pediatric patients emerge. Visit LiVDerm’s Atopic Dermatitis Digital Education Hub to access a number of complimentary resources for both practitioners and patients.